As we continue to face episodic COVID surges globally, the U.S. government and its Centers for Disease Control need to focus on enhancing our systems for detecting the next highly infectious variant before we are caught unprepared once more. To do this, our government needs to invest in technology and fix current systemic inefficiencies to rapidly sequence the genetic information of COVID variants so that doctors and public health officials are better able to inform the public and strategize accordingly for implementing control measures.
The importance of genomic sequencing, a method to analyze the “genetic fingerprint” of the circulating strain, has been clear during the pandemic, and the U.S. should be learning from efforts it has helped fund—including the President’s Emergency Plan for AIDS Relief (PEPFAR) and other multinational partnerships through the United Nations—in other parts of the world. In Botswana and South Africa, a long history of genetically sequencing HIV, and deploying public health workers to gather samples and trace contacts, set both countries up to rapidly understand emerging SARS-CoV-2 variants such as Omicron.
In South Africa, public health officials noted rising case numbers in two cities, and through sequencing samples, technicians found an unusual characteristic in the viral genome: one of the target genes, the S gene, didn’t show up in the tests despite being present in the virus sample. This characteristic had previously only been seen in variants in other regions of the world, alerting experts that something was different. Similarly, in Botswana, weekly surveillance testing picked up an unusual sequence in a set of samples that was then quickly traced to travelers on a diplomatic mission.
Both countries had already established and formalized networks of genomic surveillance, which included random weekly sampling from all regions of the country. This involved working with all molecular testing labs and frontline health teams to regularly sample people who were suspected of, or had tested positive for, COVID, and investigating outbreaks and sampling points of entry. By working in close partnership, scientists in Botswana and South Africa’s Network for Genomic Surveillance were able to quickly sequence Omicron’s RNA and disseminate information around the globe about the unique qualities of this variant.
Conversely, the U.S. has struggled significantly with genomic sequencing, as a consequence of massive fragmentation, in which state, private sector and academic laboratories are working in parallel or in isolation from one another, and of long-term underinvestment in our own public health system.
This has led to relatively slow detection of new outbreaks and new strains. More recently, the widespread use of rapid antigen tests at home has resulted in many positive samples never reaching a lab for further sequencing.
The CDC attempted to address shortcomings early on by establishing the SARS-CoV-2 Sequencing for Public Health Emergency Response, Epidemiology, and Surveillance (SPHERES) consortium in May 2020 to coordinate SARS-CoV-2 sequencing and created a collaborative network among state laboratories, academic institutions, nonprofits, private sector companies and international collaborators. In 2020 and 2021, SPHERES funded a number of institutions to work on improving surveillance across several states. Despite this, there is still much work to be done.
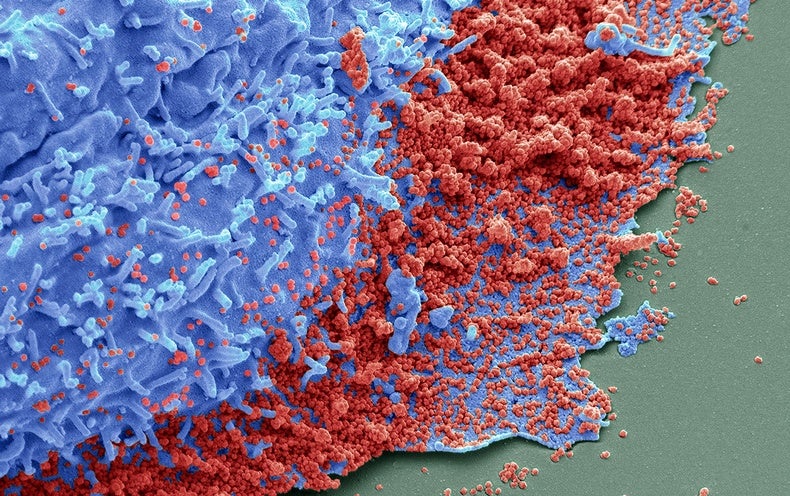
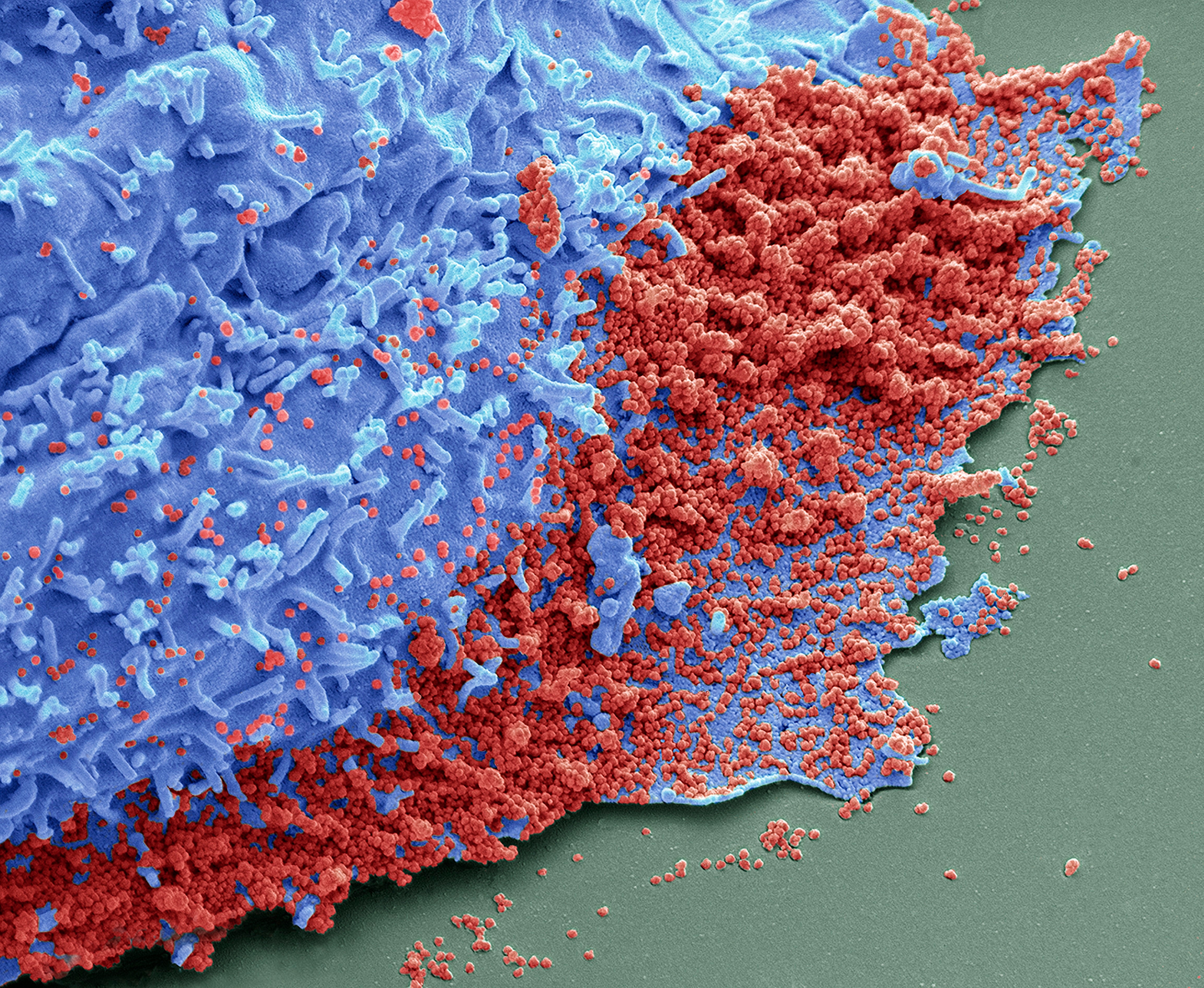
Genomic sequencing, a laboratory method used to determine the genetic blueprint of an organism or cell, has several critical applications that have been used throughout the pandemic. Primarily, it allows scientists to trace how viruses change over time by identifying mutations the virus makes in its genetic information as it moves from host to host (or, in some cases, as it continues to replicate within a single host for a long period of time). Most of these mutations are not consequential; they do not make it easier for the virus to survive, or infect, or replicate itself. But some of these mutations do make a difference; they affect how the virus enters cells, how it escapes the body’s immune response, how it becomes resistant to certain medications, and replicates.
These are the ones, like those found in the Delta and Omicron strains, that become variants of concern.
Gathering this information is critically important to understanding when it may be time to sound the public health alarm. Through sequencing, Southern African scientists discovered that Omicron has over 30 mutations in the spike protein, the part of the virus particle that allows it to bind and enter into cells. Some of those mutations are part of why Omicron is highly transmissible, moving easily from one person to the next. We now think that Omicron’s ability to evade the immune response is key to its increased transmission.
Other information that genomic sequencing gives us includes whether newer variants can possibly evade detection from molecular diagnostic tests, or whether they have reduced vulnerability to therapeutics, such as antivirals or monoclonal antibodies (which has been the case with Omicron).
Another important aim of sequencing is to better understand and explain how the virus spreads from person to person—what is called “chains of transmission.” Recently scientists used sequence data from multiple samples of infected people to show that a traveler in a quarantine hotel in Hong Kong likely infected the person in the room across the hallway via airborne transmission of the Omicron variant.
Genomic sequencing has already helped parts of the U.S. track this virus. Last summer, the Massachusetts Department of Public Health worked with the Harvard Broad Institute to analyze the famous Provincetown outbreak that showed vaccinated people were still at risk of infection and transmission. This ultimately led to a renewed effort to reinstate mask-wearing throughout the state.
Genomic sequencing also enables scientists to determine where and how new lineages of the virus came to be. In the case of Omicron, this divergence on the evolutionary tree likely occurred in mid-2020. Through sequencing, scientists determined that the Omicron variant was highly mutated and looked significantly different from Alpha, Delta and other known SARS-CoV-2 variants. The genetic data also suggest that Omicron had continued mutating from its point of divergence, either in a human or animal host, without causing an epidemic surge until one unfolded earlier this year. One theory is that the variant emerged from an immunocompromised person whose immune system could not clear the virus, allowing it to mutate for long periods of time. This data could help improve pandemic prevention by better targeting and sequencing samples from immunocompromised patients in the future, as one example.
But overall, the U.S.’s epidemic response has suffered from poor coordination of genomic sequencing. In the beginning of the epidemic, there were no federal mandates, increases in funding or even a coordinated national response focused on sequencing the genomes of the viruses we were isolating from people who were sick. In February 2021, one year into the pandemic, the U.S. CDC infused $200 million into sequencing efforts, with the promise of more support through President Biden’s American Rescue Plan.
As of early December 2021, the country was sequencing 14 percent of all PCR diagnostic tests. This was a significant increase from January 2021, when it was less than 1 percent, but there were still delays of several weeks between sample collection and results, as well as wide differences in the scale of sequencing across states. This meant there were large pockets of the country where it was not possible to detect a new variant quickly.
One important way to improve surveillance efficiency would be to utilize screening assays that do not rely on whole genome sequencing—such as the S gene target failure (SGTF) technique used to identify Omicron—to rapidly focus our sequencing technologies on samples that are more likely to represent new strains.
The detection of the Omicron variant highlights the importance of having a strong genomic surveillance system in place that can function across the silos of academia, clinical medicine and public health—which will be important not only for the next SARS-CoV-2 variant but also for the next pandemic virus. We urge the CDC and the federal government to not overlook the importance of rapid surveillance as Congress battles over funding. As we have learned from this pandemic, with one million Americans dead, it’s hard to fight an enemy that we don’t fully understand.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.